Medical Staff News
 Annual Mandatory Education
Annual Mandatory Education
Annual Provider Training for all Medical Staff (Faculty, Advanced Practice Professionals, Residents, Fellows and Students) at Harris Health must be completed yearly in order to adhere with regulatory requirements. The 2022 training will become available on March 1, 2022 with a completion deadline of May 31, 2022.
The training curriculum is completed online via Harris Health’s Learning Management System (LMS), SABA. Please allot 2-3 hours to complete this education. New for 2022, you may complete this from your mobile device.
Individuals that do not meet the deadline will have their Epic inactivated. They cannot provide any patient care at Harris Health, including supervision of House Staff.
Thank you for your compassionate care of our communities.
Quality & Patient Safety Update
 Code Stroke
Code Stroke
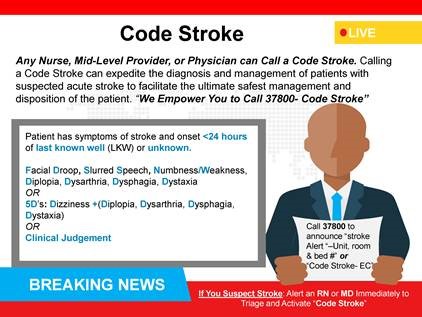
Any nurse, midlevel provider, or physician can call a Code Stroke. Calling a Code Stroke can expedite the diagnosis and management of patients with suspected acute stroke to facilitate the ultimate safest management and disposition of the patient. “We empower you to call ext. 3-7800 – Code Stroke.”
When?
When a patient has symptoms of stroke and onset is <24 hours of last known well (LKW) or is unknown.
Symptoms:
Facial droop, slurred speech, numbness/weakness, Diplopia, Dysarthria, Dysphagia, Dystaxia
OR
5Ds: Dizziness + (Diplopia, Dysarthria, Dysphagia, Dystaxia)
OR
Clinical Judgement
If you suspect a stroke, alert an RN or MD immediately to triage and activate “Code Stroke.”
Call ext. 3-7800 to announce “Stroke Alert” – Unit, Room and Bed #” or “Code Stroke – EC”
Click here for a printable file.
 A High Reliability Organization Principle
A High Reliability Organization Principle
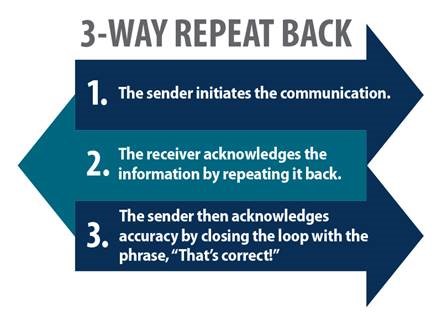
The 3-way repeat back principle is a proven effective communications practice that assures understanding between communication sender and receiver.
Patient safety champions use this communication method daily to assure clinical handoffs and procedures continue to be of high quality and focused on patient safety.
 Physician Efficiency Tips
Physician Efficiency Tips
Change the Order of Your Inbasket Folders
To make it easier to find important or frequently used folders, you can move them to the top of the list.
- On the In Basket toolbar, click
 Preferences.
Preferences. - In the window that appears, go to the Folder Order tab.
- In the Other Folders section, click
 next to your most frequently used folders to move them to the My Favorites section. Or, drag them up to that section.
next to your most frequently used folders to move them to the My Favorites section. Or, drag them up to that section.
• To remove a folder from the My Favorites section, click  or drag it back to the Other Folders section.
or drag it back to the Other Folders section. - Drag and drop to rearrange the folders in the My Favorites section. When these folders contain messages, they appear at the top of the folder list pane in the order you've specified.
• The remaining folders continue to appear in the default display order below the folders you've moved to the top. - Click Accept to save your preferences.
 Research Spotlight
Research Spotlight
Lyndon B. Johnson Hospital Division of General Surgery
By Lillian Kao, MD
The McGovern Medical School Department of Surgery has an active clinical research program at Lyndon B. Johnson Hospital (LBJ) that has steadily increased its scope in the past 15 years. The research team has completed multiple clinical studies, including randomized trials focused on gallstone disease, hernias, and acute appendicitis. LBJ is one of a number of hospitals that participates in multi-center trials funded by the Patient Centered Outcomes Research Institute (PCORI) addressing common surgical problems. For example, LBJH was a site for the Comparison of Outcomes of antibiotic Drugs and Appendectomy (CODA) trial, the largest randomized trial ever completed comparing medical to surgical therapy for acute appendicitis. As a result of this trial, individualized counseling can be offered to patients for shared decision-making regarding treatment of appendicitis, and this tool is available in both English and Spanish.
Other studies from the surgical research team have addressed disparities in surgical care for underserved patients. For example, Dr. Curtis Wray has published on disparities in cancer care and was the recipient of a career development award from the American Cancer Society to evaluate the effects of early palliative care referral on outcomes of patients with advanced hepatocellular carcinoma. Dr. Krislynn Mueck, a current acute care surgery fellow and future faculty, is pursuing research on improving health literacy in surgery patients, a focus which will certainly benefit the LBJ patient population.
Over the years, research in the Division of General Surgery at LBJ has nurtured the development of junior surgeon scientists and trainees. In the last 20 years, four LBJ faculty have had career development awards. In addition, Dr. Julie Holihan, Assistant Professor of Surgery, currently has a NIH career development award from the Center for Clinical and Translational Sciences at McGovern Medical School. Her research focuses on assembling the evidence base to inform shared decision-making around the management of asymptomatic or minimally symptomatic inguinal hernias. In addition to developing faculty, the division has also supported numerous students and residents in research training. Trainees have collectively published in peer-reviewed journals and presented at numerous locoregional and national meetings including at the prestigious American Surgical Association.
The vision for the division at LBJ is to grow surgical research to further inform and improve the care of our vulnerable patient population, to ensure diverse representation of patients in important multi-center clinical trials, and to highlight the outstanding work that is being done at LBJ and in the Harris Health System. Under the leadership of Dr. Tien Ko (Chief of Surgery, Chief of Staff, LBJ), Dr. Jonah Stulberg (Vice-Chair of Research, Department of Surgery), and Dr. Michael Wandling (Director of Surgical Research, LBJ), the research program is growing to include more collaborative efforts between departments, schools, and institutions. The division is poised to be a leader in surgical research and education in the years to come.
Physician Kudos
 Ben Taub Hospital
Ben Taub Hospital
“Everything was good, especially Dr. Kayani. He is the best doctor, and because of him I was able to do my procedure. God always blesses him!”
— BT 4E Trauma/Surgical ICU
 Lyndon B. Johnson Hospital
Lyndon B. Johnson Hospital
“Yes, Dr. Prater treated me with care and respect, and I feel 100% better today than when I went in the other day. Thank you!”
— LBJ Emergency Center
 Ambulatory Care Services
Ambulatory Care Services
“Hello. I wanted to leave my feedback on Dr. Challa. She was great — very helpful, very caring. She cared about all of my needs, and explained everything to make sure that I got my referrals for my follow up with my psychiatrist. She's awesome and she really cares about people, I can tell. She just doesn't do it for a check. She actually loves people and loves caring for people. She's a great person and may God bless her and her family.”
— Martin Luther King Jr. Health Center
Thank you for your service!