
Harris Headlines
True to form, the CDC and Austin continue to keep us on our toes! Amazing to think that at this time last year, we were having to reprocess masks. Now, while we still mask up in the hospital and clinics with plenty of PPE, we are given permission to forego masks in our private lives, if we are fully vaccinated. We are safer and more protected. What a relief after the past 14 months!
Thank you for standing firm during what will likely be the most remarkable public health crisis through which most of us will work in our lifetime. Francis Weld Peabody famously said, “One of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient.” Individually and collectively you have dedicated your daily work to humanity and to caring for each patient. Again, thank you.
As promised, this month I will highlight the second Pillar of the new Harris Health Strategic Plan: People. This pillar is not only focused on the patients served by Harris Health, but also the people who come to work every day to live out the Harris Health mission. You. Physician satisfaction and engagement are critically important the strength and success of Harris Health. Physicians are leaders throughout the health system and the creation of more opportunities for physicians to provide input, drive change, and influence decisions are key to transforming the health of Harris County. Below you will see a snapshot of Pillar 2.
Executive sponsors of Pillar 2 include the SVP of Human Resources, the Chief Nursing Executive, and the hospital chiefs of staff, Drs. Tien Ko and Sandeep Markan.
Safe at Harris Health
Clinical alarms are intended to warn caregivers of immediate or potential adverse patient conditions. However, the steadily increasing use of alarm-equipped medical devices has presented caregivers with a dizzying array of alarms to manage which can lead to alarm fatigue. When alarms are not managed effectively, patient safety can actually be compromised.
Because patient safety is paramount to our mission, Harris Health has formed a Clinical Alarm Management Program to improve the effectiveness of clinical alarms. The first step in this process was to form a Quality Assurance and Performance Improvement (QAPI) Alarms Management Group. The QAPI Alarms Management Group is a multidisciplinary team, which includes key stakeholders from our medical and nursing leadership, quality, patient safety and risk management, biomedical engineering, and IT staff. Drs. Jennifer Chen, Joey Fisher, and John Foringer represent the medical staff.
This group will be responsible for assessing our current management of alarm systems, identifying areas for improvement, and implementing any changes in technology, policies, or procedures necessary to ensure clinical alarm safety.
Members of the QAPI Alarms Management Group may visit your care areas to observe and interview staff as they identify barriers and opportunities for improvement. Your experience and expertise will truly be valuable as we embark on this initiative.
In addition, please continue to report any issues related to alarms to the eIRS. Safety is the essential job of each member of the Harris Health workforce. To become a High Reliability Organization with the goal of zero harm, this requires the support and commitment of every team member.
If you have any questions, please contact Joseph Kunisch, VP of Quality.
Dynamic Data
Correct patient identification is a critically important safety practice in healthcare systems. At Harris Health the correct method for identifying a patient is to ask “What is your name?” followed by “What is your date of birth?” When correct patient identification does not happen, errors occur. Patients may get the wrong medication, get taken to the wrong diagnostic study, or worse.
The Safety and Risk Management team receive approximately 1,000 incident reports (eIRS) each month. They categorize and monitor event trends in the system. Recently, there has been an uptick in the number of patient identification events at Harris Health.
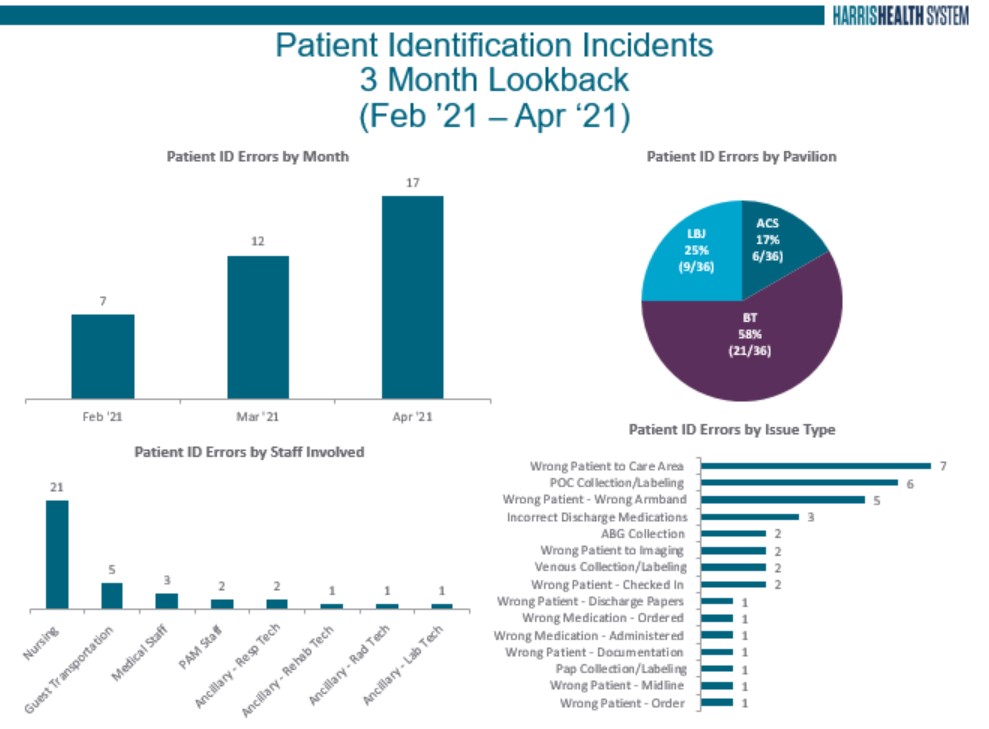
Analysis of the eIRS data has alerted leadership to the need to re-engage the health system on the topic of 2-patient identification in all care encounters. Be on the lookout for an upcoming system-wide safety campaign that focuses on patient identification as a critical element of our safety work. In the meantime, ask every patient, “what is your name” and “what is your date of birth” and teach all of your fellows, residents, and students to do the same.
Medical Staff News
Check out today’s Medical Staff Town Hall at 12:30pm.
Graduating Students, Residents, & Fellows of Baylor and University of Texas
Check-Out Process
As you prepare to leave your training program, you are required to complete the check-out process. This applies to all trainees, including House Staff Members who will become Faculty or transferring into another training program within Harris Health System.
Requirements for Exit:
- Complete and Return Check-Out Form to Medical Staff Services. Out of Contact Designee Signature is required. This may be the Attending or Chief of Service. The Check-out form may be obtained by emailing MedicalStaffServices@harrishealth.org.
- Medical Records Clearance (HIM) – Schedule a required virtual Check-out Appointment with HIM. Be sure to clear your Epic in-basket prior to your appointment. (Students Exempt)
- Return all scrubs to Harris Health Pyxis Scrub Machine or the Linen Department which you withdrew the scrubs from.
- Return Badge, Pager and Call Room Key(s) (if applicable) to Harris Health Security Office by placing them in the envelope provided to you in Security. Medical Staff Services will sign-off as received once the envelope is retrieved.
Mandatory Training
The deadline for Medical Staff, Fellows, Residents, and Medical Students is Monday, May 31st. Any staff who has not completed the training will have his/her EPIC access suspended. Suspension of EPIC access also means that the provider or trainee is not allowed to provide clinical care until EPIC access has been reinstated. Reinstatement can take up to 48 hours once the training modules are documented as complete. DO NOT WAIT. Get your training completed today.
reSEARCH
Coming Soon One of the great benefits of working in the largest medical center in the world and with top tier medical schools and academic partners is the opportunity for partnering on cutting edge research that advances knowledge and understanding of how new therapies and interventions impact diverse patient populations. Beginning with the June issue of Rounds, we will highlight ongoing research projects at Harris Health System. Stay tuned.
Care Done Well
Are you familiar with the Multi-Visit Patient (MVP) Initiative? MVPs are patients with high utilization of Harris Health's emergency centers (EC). They are patients with 10+ visits to the EC in the last year, and while they represent 0.7% of EC patients, they account for more than 8% of all EC visits. They suffer from a combination of behavioral, social, and medical conditions that drive excessive utilization of the EC.
The program, sponsored by the department of Population Health, is a collaboration between ACS, BT Hospital, LBJ Hospital, and community partners such as the Houston Recovery Center and Coalition for the Homeless. Community Health Workers (CHWs) trained in the MVP method meet MVPs in person in the EC to assess their circumstances and needs. The CHWs work with partners across the continuum of care to link the MVPs to needed resources such as housing, behavioral health services, or substance use treatment. Since these patients' high utilization is often a result of multiple complex factors, the CHWs work with the MVPs, community partners, and relevant internal resources to manage the patients over time and plan for future EC encounters, knowing that multiple attempts and persistent engagement are necessary to effect change.
EPIC functionality has been created, including an MVP banner and an MVP note to help identify MVPs and unify their care plan. These functions enable physicians, nurses, and case managers to work in collaboration with the CHWs and external partners to help our most vulnerable patients. The program now includes coordination with area hospitals to identify shared MVPs and conduct joint case conferences to advance their care plans and stabilize their utilization, thereby improving quality of care and patient throughput.