Robot-Assisted Surgery at Harris Health
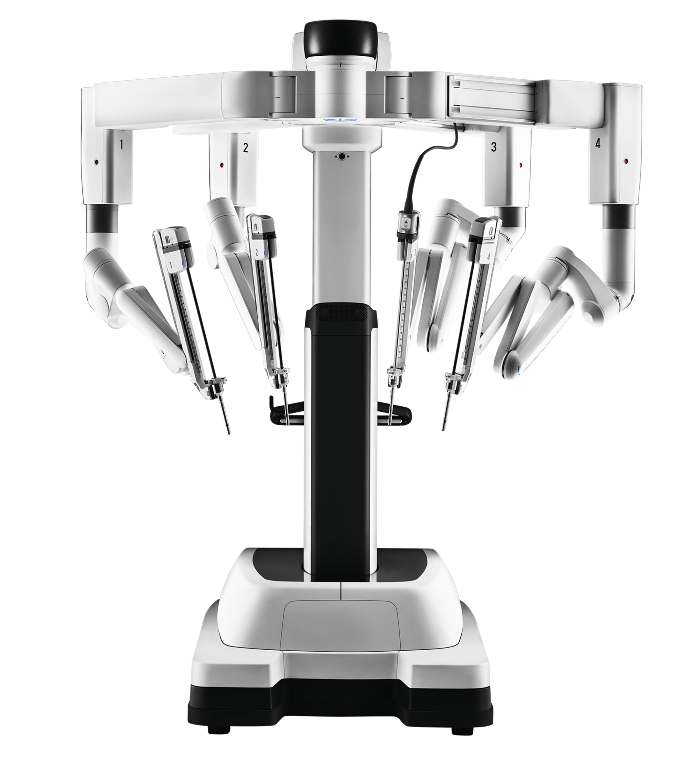
Robot-assisted surgery is now underway at Harris Health System. On Aug. 29, 2022, a general surgery case of a diversion colostomy was successfully completed as our first robotic surgery procedure in several years, and the patient was discharged the next day. This was performed by general surgeon Erik Askenasy, MD, at LBJ Hospital using the Da Vinci Xi system, a well-established model used in many academic centers nationwide.
 With robot-assisted surgery, patients will have “less pain, easier recovery and an earlier return to baseline,” says Askenasy. He cites a reduced length of stay for major colon resections, for example, from 3-5 days for open procedures, 2-3 days for a conventional laparoscopic approaches and 1-2 days for robotic-assisted procedures. With robotic surgery, all options of minimally invasive surgery are now available at Harris Health System.
With robot-assisted surgery, patients will have “less pain, easier recovery and an earlier return to baseline,” says Askenasy. He cites a reduced length of stay for major colon resections, for example, from 3-5 days for open procedures, 2-3 days for a conventional laparoscopic approaches and 1-2 days for robotic-assisted procedures. With robotic surgery, all options of minimally invasive surgery are now available at Harris Health System.
Quality Digest
The following quality and patient safety updates are specific to code blue events and central line insertions.
- Code blue events will now be documented electronically in Epic in the Code Narrator.
- The nurse will document all event interventions and medications administered into the code narrator (a nursing documentation module).
- After the nursing documentation is completed, you will receive an In-basket message to sign off on all administered medications and code report.
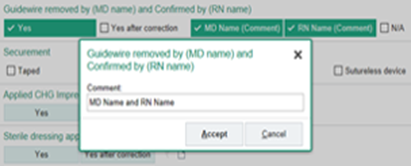
- A Central Line Insertion Checklist has been created and moved into EPIC for the nurse to complete during the central line insertion.
- Nurses must be present for ALL central line insertions in order to complete the checklist in real time.
- The checklist captures insertion related CLABSI prevention best practices with special attention given to the removal of the guidewire.
- Outside of emergent central line insertions in the EC or ICU, please coordinate timing so that a nurse can be present.
- If a nurse is not present, it is your duty to request their presence during the central line insertion.
Clinical Documentation Improvement Tip
Best Documentation Practices: Respiratory Failure
- Documentation should specify acuity-acute, acute on chronic, or chronic
- Documentation should specify type – hypoxemic, hypercapnic – (no abbreviations such as AHRF)
- Differentiate between intubation for airway protection vs. actual failure
- Ensure clinical validation for postoperative failure, especially within 48 hrs. post-op
- Document clinical indicators to support the diagnosis of respiratory failure (ABGs, P/F ratio, new oxygen requirements, or home O2)
- Identify the underlying or associated cause (COVID-19, pneumonia, COPD, trauma)
SIMPLE
ADVANCED
Remember to clinically validate your diagnosis within the medical record with justifiable, supported clinical criteria.
See examples in attached reference sheet.  Informatics Update
Informatics UpdateAttached are three important informatics updates for the Epic EHR:
Physician Recognition
Exceptional feedback from our patients about our doctors
 Asna Matin, MD
Asna Matin, MD Pediatrics
Sheldon Health Clinic
Baylor College of Medicine
“Dr. Matin is a great doctor! Very easy to talk to. She is extremely skilled at questioning her patients and obtaining necessary information without sounding like she's going through a questionnaire. She made my 16 year old daughter open up and respond positively.”
 Daniel Ostermayer, MD
Daniel Ostermayer, MDEmergency Center
Lyndon B. Johnson Hospital
McGovern Medical School at UTHealth
“From the moment I arrived, the treatment I got was amazing. Dr. Ostermayer was very thorough, and handled everything in one visit.”
 Dacia Ticas, MD
Dacia Ticas, MDEmergency Center
Ben Taub Hospital
Baylor College of Medicine
“Doctor Ticas was sweet and compassionate, and explained everything to me. I respect that. The wait was minimal which surprised me. Thanks, and I will call on you again!”
Thank you for your service!